A 35 year old man presented to the casualty with the complaints of
Bilateral pedal edema since 1 week
Dyspnea since 15 days
Abdominal distension since 2 months
History of Presenting illness
A 35 year old man, who sells plants at nalgonda tells us a detailed insight to the reason for all his problems. He says he has been married 9 years back but since the past 5 years he has been living apart from his wife and his 2 sons due to marital issues. Prior to that he used to consume alcohol occasionally but since the past 5 years he has been consuming about half to 1 bottle of whiskey everyday.
3 years back, he paid a visit to a local hospital with abdominal distension and pedal edema and he was diagnosed with chronic liver disease for which he used medications for a while and stopped. He was even diagnosed to be a diabetic back then and he started using Tab Metformin 500mg OD.
2 months back, his abdominal distension increased and his eyes became yellow after which he started using local herbal medications.
Since the past 15 days he has been experiencing dyspnea on exertion after which he paid a visit to a local hospital and they put him on certain medications which relieved his symptoms.
Since the past 1 week, he says his abdominal distension has increased and so as his dyspnea, it has increased to such a point that even at rest it isn't getting relieved.
On presentation to casualty,
He was tachypneic with icterus and a respiratory rate of 36 cpm,
Heart rate of 120 bpm, BP at 130/70mmhg and GRBS 150mg/dl
Cvs - JVP raised
Muffled S1,S2+
Lungs - Inspiratory crepts in bilateral IAA,SA
Per Abdomen - Distended
Bowel sounds +
Past illness
K/C/O type2DM since 2 years on tab mentformin 500mg
No History of hypertension, TB,Asthma
Personal history:
Diet:Mixed
Appetite:Normal
Sleep:Regular
Bowel and bladder:Regular
Addictions:The Patient has a history of alcohol intake that began 10 years ago and has been drinking 180ml of whiskey
Drug history:
On oral hypoglycemic for DM2 for 2 years(Metformin 500mg)
Family history:
No Similar Complaints in the family
General Examination:
was examined in a well-lit room, with informed consent.
Conscious and coherent and cooperative,Orienteted to time,person and place
Pallor:Absent
Icterus:Present
Cyanosis:absent
Clubbing:absent
Lymphadenopathy:absent
Edema:present(pitting type)
Vitals(at the time of admission):
Temperature:98.4F
PR:P8Bpm
RR:24cycles/min
BP:110/80 mm of hg
SpO2:96%
GRBS:155mg%
Systemic examination:
CVS:S1,S2 heard
Respiratory system:
Dyspnea present
Vesicular breath sounds heard
Per abdomen: distended
Tenderness:epigastric region
Free fluid: present
CNS:Normal
Investigations:
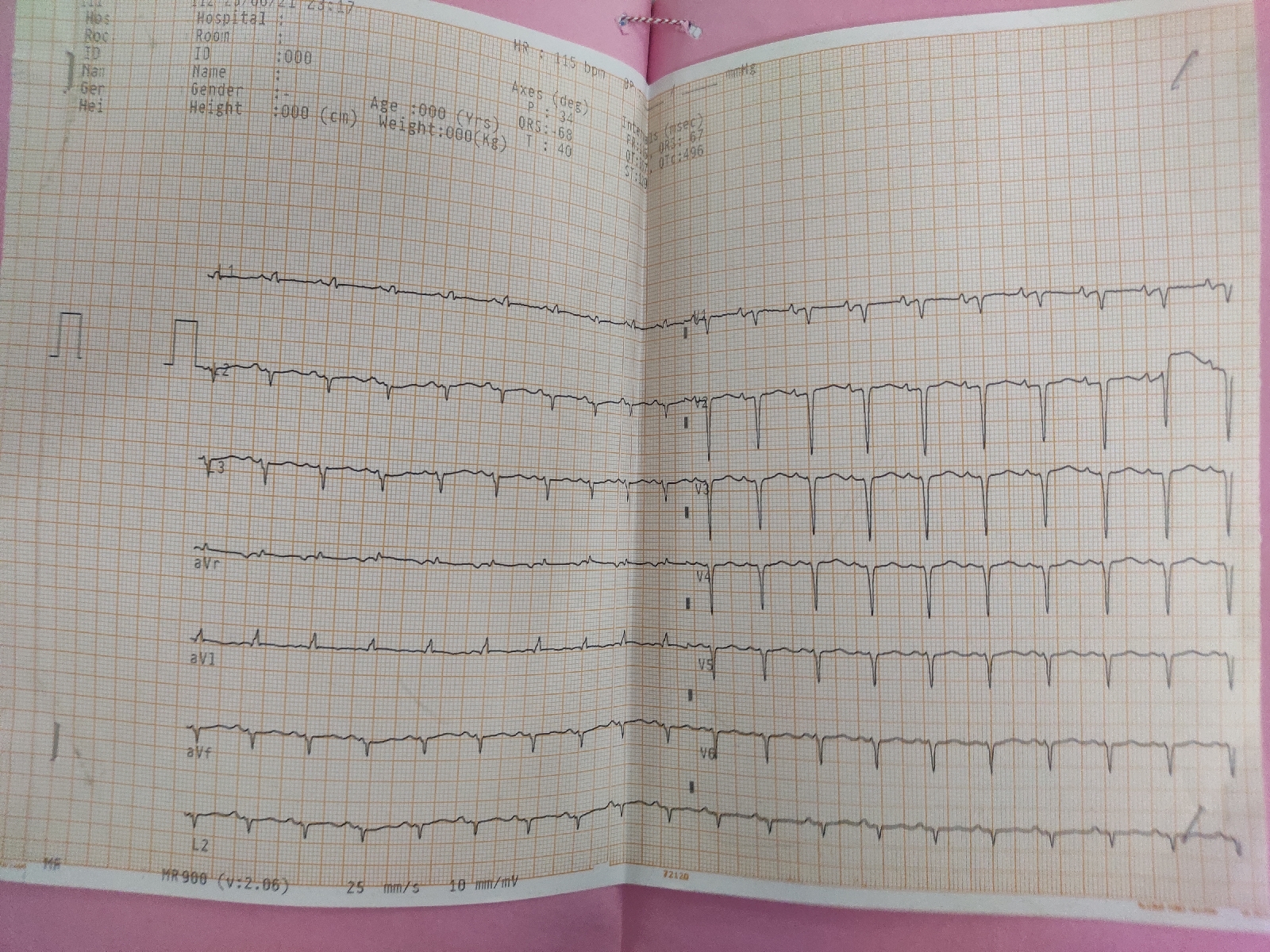
ECG:
24/06/21
26/06/21:
2D ECHO:
FBS:
Blood Urea:
S.Creatinine
APTT:
Bleeding time and clotting time:
S.Electrolytes:
Prothrombin time:
LFT:
Ultrasound
Provisional diagnosis:
Diagnosis-
1. DCMP with EF 20% secondary to alcoholism
2. Chronic Liver disease
3. Alcohol dependence syndrome
4. Known case of Type 2 DM since 2 years
Treatmennt:
25/06/21
1)Head end elevation
2)O2 supplementation(maintain Spo2>92%)
3)INJ.PANTOP 40mg iv/OD
4)TAB.UDILIV 300mg PO/BD
5)INJ.THIAMINE 20amp in 100ml NS/IV/TID
6)SYP.LACTULOSE 10ml/PO/TID
7)Maintain 2-3 stools per day
8)Fluid restriction <1liter/day
9)GRBS Charting 6th hourly
10)TAB.LASILACTONE(20/50)MG PO/BD
11)TAB.PREGABA 75 mg/PO/OD
12)NICOGUMS 2mg SOS
13)INJ.HUMAN ACTRAPID INSULIN S/C(8Am-2pm-8Pm)
14)Salt restriction <2gms/day
26/06/21
1)Head end elevation
2)O2 supplementation(maintain Spo2>92%)
3)INJ.PANTOP 40mg iv/OD
4)TAB.UDILIV 300mg PO/BD
5)INJ.THIAMINE 20amp in 100ml NS/IV/TID
6)SYP.LACTULOSE 10ml/PO/TID
7)Maintain 2-3 stools per day
8)Fluid restriction <1liter/day
9)GRBS Charting 6th hourly
10)TAB.LASILACTONE(20/50)MG PO/BD
11)TAB.PREGABA 75 mg/PO/OD
12)NICOGUMS 2mg SOS
13)INJ.HUMAN ACTRAPID INSULIN S/C(8Am-2pm-8Pm)
14)Salt restriction <2gms/day
15)TAB.MET XL 12.5mg/PO/BD
27/06/21:
1)Head end elevation
2)O2 supplementation(maintain Spo2>92%)
3)INJ.PANTOP 40mg iv/OD
4)TAB.UDILIV 300mg PO/BD
5)INJ.THIAMINE 20amp in 100ml NS/IV/TID
6)TAB.ALDACTONE 50mg PO/BD
7)Maintain 2-3 stools per day
8)Fluid restriction <1liter/day
9)GRBS Charting 6th hourly
10)TAB.LASILACTONE(20/50)MG PO/BD
11)TAB.PREGABA 75 mg/PO/OD
12)NICOGUMS 2mg SOS
13)INJ.HUMAN ACTRAPID INSULIN S/C(8Am-2pm-8Pm)
14)Salt restriction <2gms/day
15)TAB.MET XL 12.5mg/PO/BD
16)TAB.DYTOR 20mg/PO/OD
28/06/21:
1)Head end elevation
2)O2 supplementation(maintain Spo2>92%)
3)INJ.PANTOP 40mg iv/OD
4)INJ.THIAMINE 20amp in 100ml NS/IV/TID
5)TAB.ALDACTONE 50mg PO/BD
6)Maintain 2-3 stools per day
7)Fluid restriction <1liter/day
8)GRBS Charting 6th hourly
9)TAB.LASILACTONE(20/50)MG PO/BD
10)TAB.PREGABA 75 mg/PO/OD
11)NICOGUMS 2mg SOS
12)INJ.HUMAN ACTRAPID INSULIN S/C(8Am-2pm-8Pm)
13)Salt restriction <2gms/day
14)TAB.MET XL 12.5mg/PO/BD
15)TAB.DYTOR 20mg/PO/OD
Advise at discharge
1. Tab Dytor 20mg PO/OD
To be taken at 8am
2. Tab Met XL 12.5/PO/BD
To be taken at 8am and 8pm
3. Tab Aldactone 50mg/PO/BD
8am and 8pm
4. Tab Metformin 500mg/PO/OD at 8 am
5. Tab Pantop 40mg/PO/OD/BBF
At 8am
6. Tab Thiamine 100mg/PO/BD
7. Nicogums 2mg/PO/BD at 8am and 2pm and sos
8. Syrup Lactulose 10ml/PO/BD
9. Advised fluid restriction <1/day
Salt restriction <2g/day
Review after 1 week to General Medicine and Psychiatry OPD
2decho findings:
1. Global Akinetic with severe TR, Mild AE and Mild PR, Moderate MR
2. All chambers dilated with EF 20%
3. Mild to moderate PE
4. Severe LV dysfunction